New research presented at the American Heart Association’s Scientific Sessions 2024 sheds light on a troubling health trend: structural inequalities and limited access to healthy foods continue to drive up rates of heart disease and related illnesses across the United States.
 University of Richmond
University of Richmond
The findings reveal how decades-old policies, like redlining, and a rising obesity rate among specific demographics, particularly in Midwest and rural communities, are influencing rates of cardiovascular disease today. Together, these studies underscore how access to healthy food, social and economic conditions, and medical support shape the nation’s heart health risks—and why these factors are critical to changing the outlook.
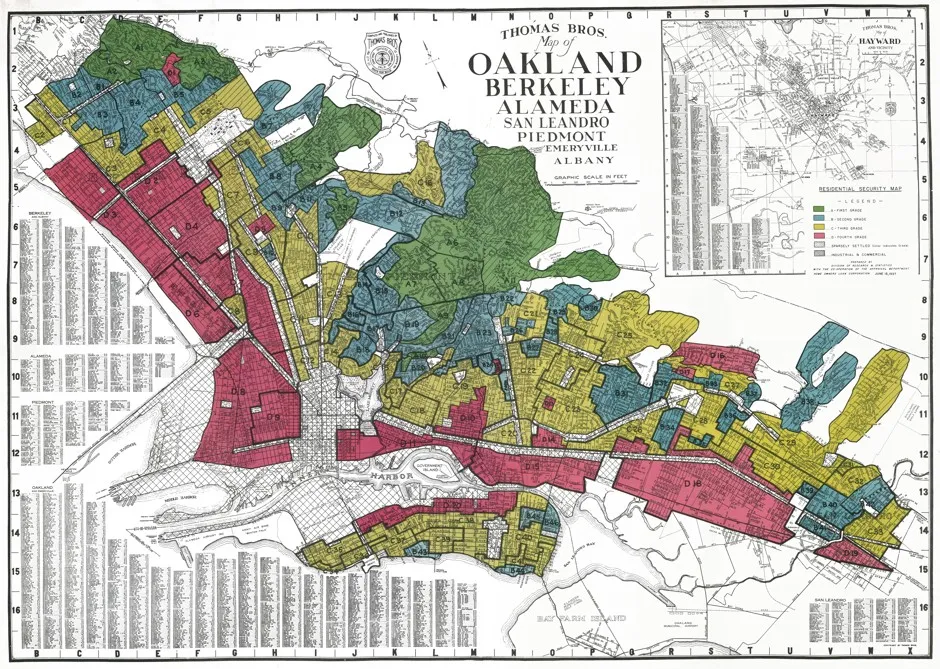
Redlining’s legacy of health inequities
One study, led by Rebekah J. Walker, PhD, of the University at Buffalo, investigated how redlining has left a legacy of health inequities in neighborhoods that still have reduced access to healthy food. Analyzing data from more than 11,000 US Census tracts across 38 states, Walker’s research found a direct correlation between redlined neighborhoods and higher rates of diet-related diseases like type 2 diabetes, high blood pressure, and coronary heart disease.
“We know that redlining leads to poor health outcomes, and even though redlining has been outlawed, it is still having an impact,” Walker said in a statement accompanying the research.
Redlining, a racially biased policy established in the 1930s, divided neighborhoods by “risk,” marking Black and immigrant communities in red, or “hazardous” zones, which shut them out of fair mortgage options. Over time, this created cycles of disinvestment and poverty, eroding local resources, including access to affordable, nutritious food.
The impact of this can still be seen today in many urban areas, where supermarkets are few and far between, forcing residents to rely on corner stores that may offer mostly processed, packaged items instead of fresh produce.
 Canva
Canva
Walker’s study highlights this lingering impact. In these redlined neighborhoods, 11.8 percent of residents had type 2 diabetes, 31.9 percent had high blood pressure, and 6 percent had heart disease. For Walker, these numbers illustrate that “many cardiovascular outcomes are diet-sensitive,” suggesting that improving access to healthier food options could reduce disease rates in these communities.
She also highlights the importance of identifying social factors, such as access to healthy foods, that may be impacted by structural racism; when structural racism affects these social factors, they can negatively impact health.
Rates of obesity-related heart disease are on the rise
In another study on the obesity epidemic’s toll on heart health, Brown University’s Aleenah Mohsin, MD, tracked a 180-percent rise in deaths related to obesity-related ischemic heart disease from 1999 to 2020.
Ischemic heart disease is a dangerous condition in which narrowed arteries restrict blood flow and oxygen to the heart, leading to a risk of heart attack. “Obesity is a serious risk factor for ischemic heart disease, and this risk is going up at an alarming rate,” Mohsin explained.
 Cottonbro Studio | Pexels
Cottonbro Studio | Pexels
The research showed that middle-aged men, Black adults, and people living in Midwestern states had the steepest increases in death rates, with the numbers underscoring the significant need for weight management, healthy diet, and preventive care.
The research highlights deaths for middle-aged men from obesity-related heart disease rose from 2.1 per 100,000 people in 1999 to 7.2 per 100,000 in 2020, a 243-percent increase. Men aged 55 to 64 experienced a 165-percent increase over the same period. Women also faced rising rates, with a 131 percent jump in obesity-related heart disease deaths.
 Getty
Getty
The trends reveal a stark reality: those living in Midwest and rural communities experienced some of the highest death rates, with age-adjusted death rates climbing to 4.0 per 100,000 in rural areas compared to 2.9 per 100,000 in urban centers. Racial disparities were also evident; Black adults had the highest age-adjusted death rates of all groups studied.
According to Mohsin, the results point to how “social and perhaps environmental factors may also be playing a significant role” in determining heart disease risks.
These findings bring new attention to the interplay between obesity, socioeconomic status, and cardiovascular health. Clyde W. Yancy, MD, from Northwestern University noted how redlining’s historical influence still shapes food access and health inequities in affected areas.
“Without question, redlining has had a negative effect on not just healthy food access but also healthy living,” Yancy explained.
“The sobering awareness is not only the persistent effect of redlining but the still evident practices which ‘de facto’ are redlining but via different means,” he added. Yancy also expressed optimism, emphasizing that community action and disruptive strategies could reduce the ongoing impact of redlining on health.
Despite these concerning statistics, both Walker and Mohsin see ways forward. The American Heart Association has promoted initiatives such as Health Care by Food, which examines the benefits of integrating healthy food as part of medical treatment.
Research limitations
Moreover, a 2022 American Heart Association policy statement advocated for “nutrition security” to ensure access to affordable, nutritious food for everyone—a step that health experts say could curb preventable diseases in vulnerable communities. Walker and her team believe this type of approach could be a powerful lever in reducing heart disease and diabetes rates by making fresh food more accessible in areas historically affected by redlining.
However, both studies acknowledge some limitations. Walker’s work, for instance, provides only an association between food access and redlining’s legacy of poor health outcomes. Meanwhile, Mohsin’s analysis focused exclusively on mortality rates from ischemic heart disease, meaning it may not reflect the true prevalence of obesity-related cardiovascular risks. These gaps underline the need for continued research into the social determinants of health, especially as heart disease remains the leading cause of death in the United States.

BECOME A VEGNEWS VIP: Get exclusive product deals, freebies, and perks galore!
Sadiya S. Khan, MD, of Northwestern University, commented on the broader significance of these findings, explaining that “the relative change in ischemic heart disease deaths related to obesity that was observed in this study between 1999 and 2020 was greater than the overall increase in obesity prevalence that we’ve seen in the United States.” Khan underscored the importance of identifying and managing obesity as a key risk factor for heart disease and stressed the need for more aggressive public health interventions.
As the American Heart Association and health advocates continue to address these gaps, improving food access and preventive care in at-risk communities remains essential. Both studies suggest that a comprehensive approach—one that addresses the roots of social inequity and promotes healthier, more accessible diets—could make a lasting difference in the fight against cardiovascular disease.
For more plant-based stories like this, read:
JUMP TO ... Latest News | Recipes | Guides | Health | Subscribe








